Abstract
Background: Follicular lymphoma (FL) is clinically and genetically heterogeneous. While most patients experience an indolent disease course, with median survival of over 15 years, a portion of patients experience early relapse and poor outcomes. The m7-FLIPI risk score has been described as a clinicogenetic method to accurately determine which patients are at highest risk for early relapse and poor outcomes (Pastore et al., Lancet Oncology 2015; Vindi et al., Blood 2015). However, molecular characterization of the m7 genes currently relies on tumor biopsies, which require an invasive procedure and may be unavailable. Furthermore, it is unclear whether the m7-FLIPI score is consistent over the course of disease. Circulating tumor DNA (ctDNA) is an emerging noninvasive biomarker for tumor detection in diverse lymphomas including FL. In this study, we evaluated the stability of m7-FLIPI status over multiple FL relapses as well as the utility of ctDNA for classification of patients with FL into high- and low-risk m7-FLIPI categories.
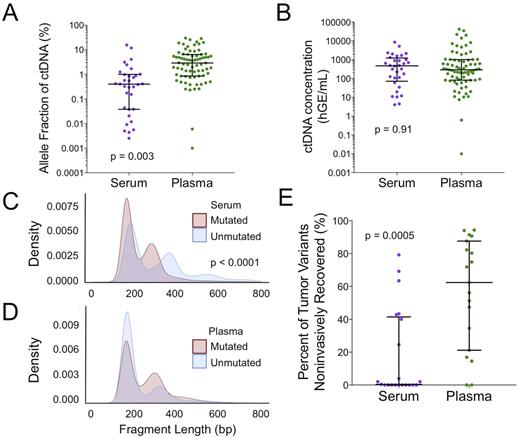
Methods: We applied Cancer Personalized Profiling by Deep Sequencing (CAPP-Seq), a capture-based method for ultra-deep sequencing (Newman et al., Nat Med 2014; Scherer et al., Sci Transl Med 2016 ) to identify risk via m7-FLIPI in pretreatment tumor and plasma samples of 29 FL patients. In addition, we retrospectively analyzed whole exome sequencing (WES) data of 37 patients from two FL cohorts (Green et al., PNAS 2015; Bouska et al., Leukemia 2017). We first validated in silico our capture-based method for identification of m7-FLIPI-relevant somatic alterations in 258 patients from the original publication (Pastore et al., Lancet Oncology 2015). We then identified non-synonymous mutations in CREBBP, EZH2, ARID1A, MEF2B, FOXO1, EP300, and CARD11 presentin each tumor and plasma sample. Using both CAPP-Seq and WES data (n = 66), we compared m7-FLIPI risk group concordance between paired diagnostic tumor biopsies, paired diagnostic and relapse tumor biopsies, paired FL and transformed FL (tFL) tumor biopsies, and paired diagnostic tumor and plasma samples. FLIPI was calculated at first FL time-point available.
Results: We observed a 95% agreement in m7-FLIPI risk category between our capture-based method and methods utilizing full exon coverage. A 100% concordance of m7 gene profile and 100% concordance of m7-FLIPI risk category were seen when comparing paired FL tumor biopsy samples from two separate lymph nodes obtained at diagnosis (n = 5). In addition, a 75% agreement in m7 gene profile and 100% agreement of m7-FLIPI risk category were observed when comparing tumor biopsy samples obtained at FL diagnosis and first relapse (n = 36; median time to relapse of 547 days, range 55 - 4200 days). There was a low concordance in m7 genetic profile between tumor biopsy samples from time of initial diagnosis and transformation (48.4%, n = 31). Importantly, concordance of m7 gene profile and m7-FLIPI risk category was 64.3% and 78.6%, respectively, when assessed by paired tumor and plasma samples obtained at FL diagnosis (n = 14; Figure 1). Furthermore, non-concordant mutations could be present in either the tumor or the plasma sample. Across all FL samples, there was no significant difference in concordance based on individual m7 genes. When analyzing pairs in which mutations were observed, concordance between paired samples was lowest for EZH2 (p = 0.028).
Conclusions: m7-FLIPI scores appear consistent between multiple FL tumor samples obtained at the time of diagnosis and across FL relapses. However, concordance in m7 gene profile between paired plasma and tumor samples is lower than between paired tumor biopsies, even at ultra-deep sequencing depths. Optimization of blood samples for assessing m7 gene profile should be performed to improve the reliability of ctDNA for determining m7-FLIPI risk status.
Figure 1. Concordance of m7-FLIPI risk category. (A) Re-classification of m7-FLIPI risk category when using paired tumor biopsy and plasma samples from 14 patients. (B) Percentage of discordant samples when comparing diagnostic tumor pairs (n = 5), diagnostic versus relapse tumor pairs (n = 37), and diagnostic tumor versus plasma pairs (n = 14). Concordance was lowest for diagnostic tumor and diagnostic plasma pairs (p = 0.013).
Diehn: Varian Medical Systems: Research Funding; Quanticel Pharmaceuticals: Consultancy; Roche: Consultancy; Novartis: Consultancy. Alizadeh: Gilead: Consultancy; Roche: Consultancy; Genentech: Consultancy; Celgene: Consultancy; CiberMed: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal